NU-664B Week 14 Assignment 1: CDC Sexually Transmitted Diseases Modules
Value: Complete/Incomplete (100 points is Complete and 0 is Incomplete)

Having Trouble Meeting Your Deadline?
Get your assignment on NU-664B Week 14 Assignment 1: CDC Sexually Transmitted Diseases Modules completed on time. avoid delay and – ORDER NOW
Due: Day 7
Grading Category: Other Assignments

Struggling to Meet Your Deadline?
Get your assignment on NU-664B Week 14 Assignment 1: CDC Sexually Transmitted Diseases Modules done on time by medical experts. Don’t wait – ORDER NOW!
Overview
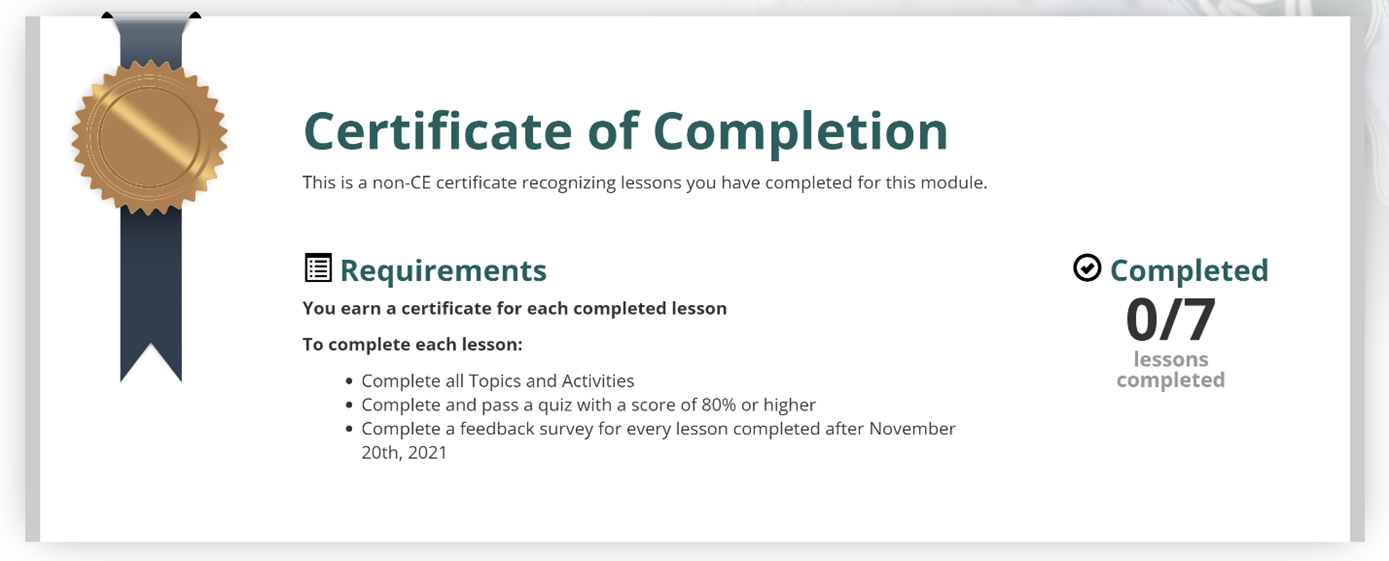
In this assignment, you will complete the following CDC Sexually Transmitted Disease modules. Upon completion of the modules this week, you are to provide a copy of your CEU certificate by uploading it to this assignment by Day 7.
The National STD Curriculum has a great deal of up-to-date information on STDs. This resource is available free of charge.
- Open STD Modules—National STD Curriculum.
- Create a free account.
- Complete the Health Professional Application for Training (HPAT).
- Complete all of the following modules: Chlamydia, Gonorrhea, Syphilis, HSV, HPV, PID, Vaginitis.
- Complete the modules and take the post-test assessments.
- Complete the evaluation form so that you can receive CNE credit.
- Submit all seven of your certificates for this assignment.
Please refer to the Grading Rubric for details on how this activity will be graded.
To Submit Your Assignment:
- Select the Add Submissions button.
- Drag or upload your files to the File Picker.
- Select Save Changes.
Submission status
| Submission status | Submitted for grading |
|---|---|
| Grading status | Graded |
| Time remaining | Assignment was submitted 5 days 12 hours early |
| Last modified | Tuesday, 4 April 2023, 11:35 AM |
| File submissions | |
| Submission comments | Comments (0) |
1. When did this episode of redness and itching start? How has it changed since it started?
The redness and itching started two weeks ago and it is getting worse
2. Did the itching start prior to the redness? (Dunphy, 2019)
I noticed that when my son started itching and scratching his skin, the area became red and inflamed
3. Is this episode like previous episodes he has had? How is it different?
I want to admit that it has gotten worse since last time. My son seems to be more irritable this time
4. Does Taumi have any known environmental, seasonal or food allergies? (Howe, 2022)
I found that any citrus fruits, tomatoes, or strawberries make him itchy. He also has seasonal allergies
5. Do you have hard water in your home? (Howe, 2022)
I am not sure, we just moved to a new house, but I will find out about it
6. How often does Taumi bathe? (Maaks et al., 2020)
Taumi loves taking a bath. He takes a bath almost everyday
7. Tell me about Taumi’s living situation such as how many siblings, does he share a room? Would he have been sharing clothing or towels with anyone? (Maaks et al., 2020)
Taumis is the only child that we have, and he sleeps in his own room.
8. Do any other close contacts have the same redness (Maaks, 2020)
I know for sure that whenever he touches our cat he sneezes
9. Do you have pets in the home? (Howe, 2022)
We have a lovely white cat
10. Has there been any recent travel history?
We took Taumi to Disneyworld in Orlando a month ago
11. Any exposure to farm animals? (Howe, 2022)
My sister-in-law has a farm, and we go to see her every other month.
12. Has Taumi had any recent infections including Strep throat? (Howe, 2022)
He hasn’t had any
1. Atopic Dermatitis (AD) – is an inflammatory condition of the skin that tends to be chronic in nature and characteristically is very pruritic. It is frequently seen in children and has higher prevalence in those with personal or family history of IGE mediated diseases including asthma and allergies (Howe, 2022). Additionally, with itching being the primary manifestation it often precedes a rash. In this case, Taumi’s mother reports his itching started first. Also, Taumi has both a personal and family history of asthma, as well as food allergies. It is further noted in this case that Taumi has experienced the same pruritic symptoms in the past with recurring skin infections. Mom also reports that Taumi is very irritable with this occurrence of symptoms. A hallmark symptom of AD is extreme pruritis which causes distress to the patient (Dunphy, 2019). Taumi’s age history of recurring episodes and distribution of his rash further correlate with a diagnosis of AD. AD often starts in infancy and is distributed primarily to the face with some diffuse patches over the rest of the body. As children get older the distribution tends to change to flexural surfaces (popliteal and antecubital spaces) (Dunphy, 2019), such as in the case of Taumi. Diagnosis of AD typically is made based upon clinical presentation, history of asthma, and involvement of skin creases including those around the eyes, as seen in Taumi’s objective examination showing Dennie Morgan lines (Howe, 2022).
2. Allergic Contact Dermatitis (ACD)- another inflammatory skin condition and is characterized by a T-cell mediated delayed hypersensitivity (Yiannias, 2021). The hallmark sign of ACD is pruritis, similar to AD. Repeated exposure to allergens is a predisposing factor. Taumi’s mother reports that they have a cat and every time he pets the cat, he becomes itchy it may be reasonable to assume that he has a sensitivity to pet dander. It is also noted that Taumi frequently visits a family farm, where he may also be exposed to allergens repeatedly. Further, ACD occurs due to exposure to personal products such as bath soaps and shampoos. Taumi’s mother did endorse very frequent baths. It should be questioned if he may have sensitivities to some of his bath products as well. ACD often has a similar eczematous appearance to AD and patients with ACD often report a history of asthma and AD (Yiannias, 2021). Therefore, ACD should be considered in the differential for Taumi. In addition to clinical presentation and history taking, patch testing can play an important role in diagnosis and identification of specific allergens.
3. Psoriasis – a multisystemic inflammatory condition, can have a variety of presentations. In addition to the common plaque psoriasis, there are other types that include guttate which present as multiple small plaques as well as pustular and erythematous forms. While this is a less likely diagnosis, it should be considered in the differential because of its close association with comorbid conditions such as psoriatic arthritis. Psoriasis is more common in adults however can present in people of all ages. Additionally atopic dermatitis may at times take on a psoriasiform appearance (Dunphy, 2019). Inverse psoriasis characteristically occurs at flexural surfaces. Taumi is experiencing itching and redness of his popliteal and antecubital spaces. Furthermore, Taumi’s mother reports concerns that his symptoms have worsened which is also a common presentation in patients with psoriasis (Dunphy, 2019). In addition to history and physical exam, skin biopsy can be used to make a diagnosis of psoriatic lesions (Feldman, 2022).
4. Scabies – is a mite infestation of the skin. It is characterized by severe itching which worsens at night. The intense pruritis of a scabies infestation is a result of a delayed hypersensitivity reaction to the mite itself or its feces or eggs (Goldstein & Goldstein, 2022). In this case it is noted that Taumi’s symptoms worsen in severity at night. While this is probably the least likely diagnosis it should be considered because of the risk of transmission to other members of the household. Dermoscopy examination for the presence of mites, feces or eggs will aid in diagnosis as well as skin scraping with microscopic examination of KOH prepared slide.
Diagnosis: Atopic Dermatitis
Plan:
Pharmacology:
• Triamcinolone Acetonide cream 0.1% – apply a thin layer to affected areas twice daily for two weeks. Do not apply to neck or face. (Follow up in two weeks to assess need for continued tx or need for systemic therapy)
• Benadryl 25 mg 1 tablet po q hs prn itch. May give one additional 25 mg dose during the day as needed for itch.
• D/C Zyrtec
• D/C Hydrocortisone cream
Non-Pharmacology:
• Maintain skin hydration – may continue using Aquaphor Ointment or other emollient. Apply to skin immediately following bath or shower and reapply as needed throughout the day to maintain hydration.
• Use only tepid water for bathing
Labs/Diagnostics:
- CBC
- Chem 4
- Uric Acid
- ESR
- skin patch testing (allergist)
- Dermoscopy
- Skin scraping and KOH prep slide
Referrals:
• Allergy Clinic referral for skin patch testing/allergen identification to aid in management of atopy
Patient Education:
• Atopic dermatitis (AD) is the most common type of eczema. It often appears as a red, itchy rash or dry, scaly patches on the skin. AD usually begins in infancy or childhood but can develop at any point in a person’s lifetime. It commonly shows up on the face, inside of the elbows or behind the knees, but it can appear anywhere on the body
• You can’t catch atopic dermatitis or spread it to others.
• avoid excessive skin dryness and irritation – keep skin moist using emollients, as a substitute for soap
• bathe using tepid water, pat skin dry and immediately treat skin with emollients
• keep bath time short to avoid removal of the skin’s protective oils
• do not use bath soaps containing perfumes or coloring agents, use on glycerin soaps if soap has to be used.
• Monitor for signs of bacterial infection (areas of redness with streaking and warmth or swelling, fevers, lethargy)
• Prevent exacerbations by avoiding triggers such as dust, dander, and pollen
• Avoid sleeping in warm occlusive clothing
• Keep all living areas at a cool temperature
• Keep fingernails short to avoid trauma from scratching
Follow Up:
• Office visit in 2 weeks to assess for improvement or need for continued therapy or changes to current therapy. Call the office sooner if symptoms worsen or you have questions or concerns regarding treatment.
Secondary Prevention: Proper skin care
• Patients with AD are at higher risk of developing colonization by staphylococcus aureus. This colonization can worsen the skins barrier function, lead to proliferation of B and T cells, and increase production of interleukin 31 which in turn induces inflammation and itch in patients with AD. Proper hydrating skin care is essential to preventing staph aureus infection in patients with atopic dermatitis.
Social determinants of health:
• There are significant disparities among different ethnicities when it comes to conditions of atopy such as asthma and eczema. Black and Hispanic patients experience higher rates of ER visits and hospitalization for these conditions when compared to non-Hispanic, whites. Additionally, those who fall under the category of low income have higher rates of ER visits and hospitalizations than those with higher income. Severe eczema symptoms are reported in those who lack insurance or are underinsured. Delays in care may be noted in persons of color when examining clinicians lack experience and training in diagnosis of skin conditions in persons of color.
References:
Dunphy, L., Winland-Brown, J., Porter, B., & Thomas, D. (2019). Primary care: Art and science of advanced practice nursing – An interprofessional approach. (5th ed.). F.A. Davis.
Feldman, S. (2022).Psoriasis: Epidemiology, clinical manifestations, and diagnosis. Up to Date. Retrieved From https://www-uptodate-com.regiscollege.idm.oclc.org/contents/psoriasis-epidemiology-clinical-manifestations-and-diagnosis?search=psoriasis&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
Goldstein, B., Goldstein, A. (2022).Scabies: Epidemiology, clinical features, and diagnosis. Up to Date. Retrieved From
https://www-uptodate-com.regiscollege.idm.oclc.org/contents/scabies-epidemiology-clinical-features-and-diagnosis?search=scabies&source=search_result&selectedTitle=1~99&usage_type=default&display_rank=1
Howe, W. (2022).Atopic dermatitis (eczema): Pathogenesis, clinical manifestations, and diagnosis. Up to Date. Retrieved From
https://www-uptodate-com.regiscollege.idm.oclc.org/contents/atopic-dermatitis-eczema-pathogenesis-clinical-manifestations-and-diagnosis?search=eczema%20children&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=2
Yiannias, J. (2021).Clinical features and diagnosis of allergic contact dermatitis. Up to Date. Retrieved From https://www-uptodate-com.regiscollege.idm.oclc.org/contents/clinical-features-and-diagnosis-of-allergic-contact-dermatitis?search=atopic%20dermatitis%20children&topicRef=1729&source=see_link
